Pediatric oncology
Pediatric oncology R+D(I+D+i )
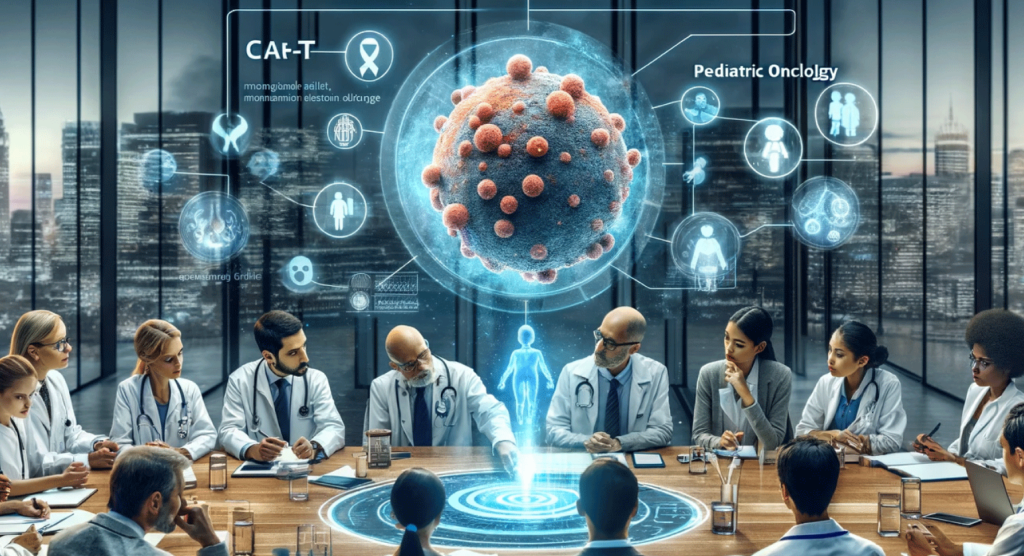
The field of pediatric oncology is witnessing significant advancements through research in CAR-T (Chimeric Antigen Receptor T-cell) therapies, a pioneering form of immunotherapy.
CAR-T therapy is a type of treatment used in certain cancers, particularly some forms of leukemia and lymphoma. It’s a form of immunotherapy where a patient’s T-cells are modified in a laboratory to attack cancer cells. The process involves extracting T-cells from the patient, genetically engineering them to produce special structures called chimeric antigen receptors (CARs) on their surface, and then infusing these modified T-cells back into the patient.
In children, CAR-T therapy has been particularly successful in treating acute lymphoblastic leukemia (ALL), which is the most common cancer in children. This therapy is considered when other treatments, like chemotherapy and bone marrow transplants, have not worked or when the cancer has relapsed.
CAR-T therapy represents a significant advancement in pediatric oncology with promising results, but it’s also associated with serious risks and limitations. The ongoing research aims to enhance its efficacy and safety profile, making it a more viable option for a broader range of patients.
The scientific exploration in CAR-T therapy area encompasses several critical aspects:
Molecular Targeting
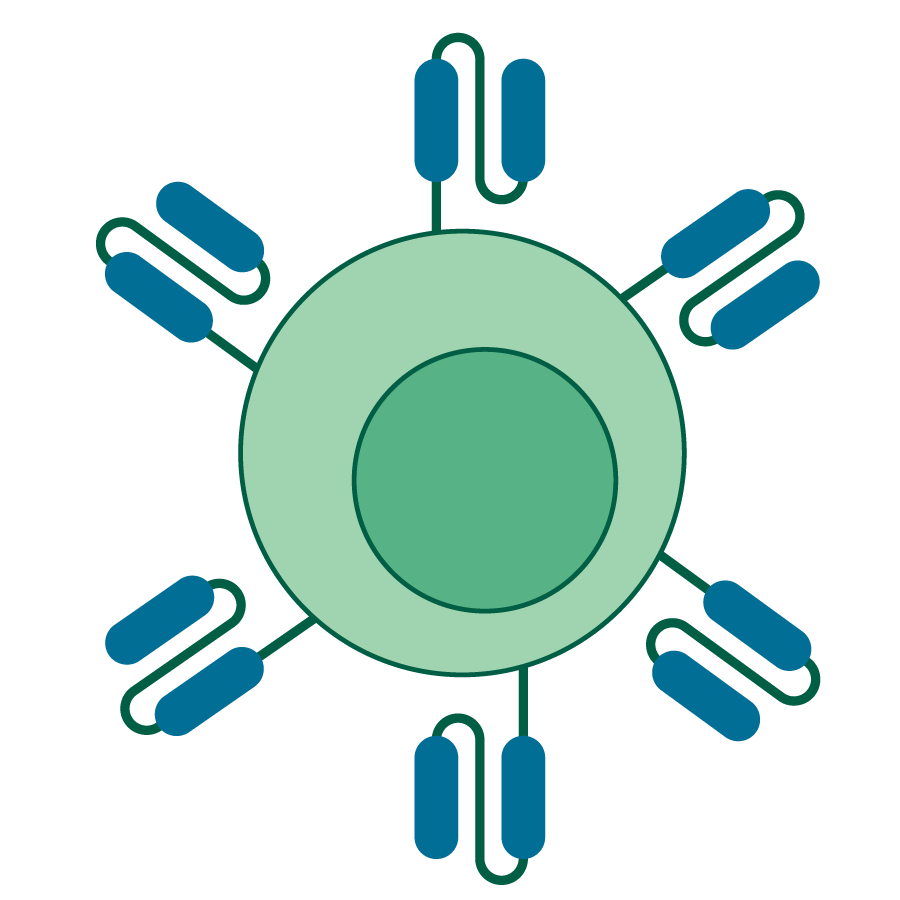
Pediatric cancers often exhibit different molecular profiles compared to adult cancers. Research is focused on identifying specific antigens present in pediatric cancers that CAR-T cells can target, ensuring the therapy’s effectiveness and specificity.
Safety and Tolerability
Given the heightened sensitivity of children’s developing bodies, a major area of research is optimizing CAR-T therapy to minimize adverse effects, such as cytokine release syndrome (CRS) and neurotoxicity, which are particularly concerning in younger patients.
Mechanisms of Resistance
Some pediatric cancers show initial responsiveness to CAR-T therapy but later develop resistance. Investigating the cellular and molecular mechanisms behind this resistance is crucial for developing more durable and effective treatments.
Expanding Indications
While CAR-T therapy has shown success in treating certain pediatric leukemias, research is underway to expand its use to a wider range of pediatric cancers, including solid tumors, which pose unique challenges due to their microenvironment and tumor heterogeneity.
Personalization of Therapy
Research is increasingly focusing on personalized approaches, where CAR-T cells are engineered to target the specific characteristics of an individual patient’s cancer, enhancing efficacy and reducing the risk of relapse.
Manufacturing Innovations
Simplifying and accelerating the CAR-T cell manufacturing process is a key research area. This includes developing standardized, scalable, and cost-effective production methods suitable for pediatric applications.
Long-Term Impact Study
Given the relatively recent introduction of CAR-T therapy in pediatrics, long-term follow-up studies are essential. These studies assess the therapy’s impact on growth, development, and overall health outcomes in pediatric patients
Collaborative Clinical Trials
International and multi-institutional collaborations are integral to this research, pooling resources, expertise, and patient populations to conduct comprehensive and diverse clinical trials.
Ethical Considerations
Research in pediatric CAR-T therapy also navigates ethical complexities, ensuring informed consent and considering the implications of involving children, who may not fully grasp the nature of the treatment, in clinical research.
Data-Driven Approaches
Utilizing advanced computational tools and big data analytics aids in better understanding patient responses, predicting outcomes, and tailoring treatment protocols based on extensive data analysis.
CAR-T Therapy – Children Benefits
- High Efficacy in Certain Cancers
CAR-T therapy has shown remarkable success in treating certain types of pediatric leukemia, particularly B-cell acute lymphoblastic leukemia (B-ALL). - Targeted Treatment
It’s a targeted approach that uses the body’s own immune cells, engineered to fight cancer cells, potentially offering a more precise treatment than traditional chemotherapy.
- Reduced Long-term Side Effects
Unlike treatments like radiation, CAR-T therapy may have fewer long-term side effects, as it’s more targeted in its approach. - Potential for Durable Remission
There’s evidence suggesting that CAR-T therapy can lead to long-term remission in some pediatric patients.